TEAR-BASED POINT-OF-CARE (T-POC) QUANTITATIVE TESTING PLATFORM
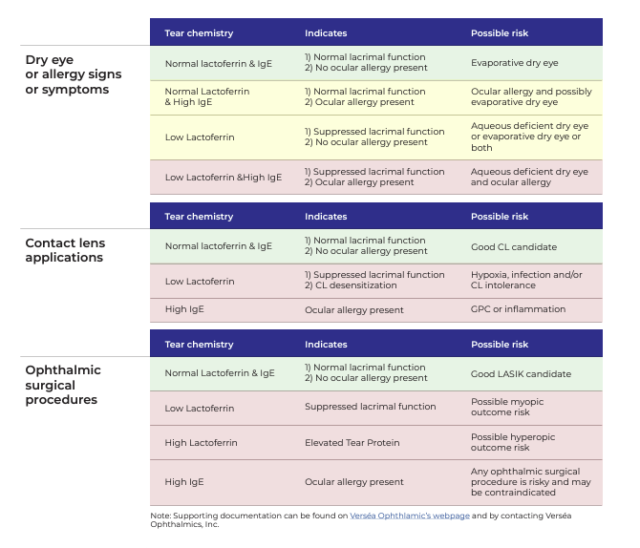
The T-POC Quantitative Testing Platform, exclusively from Verséa Ophthalmics, is being used to improve patient care in the areas of dry eye, ocular immunology, ocular allergy and ocular surgery, including LASIK. The tests are simple to perform, accurate, rapid, repeatable and reimbursable.
With the T-POC quantitative testing platform, exclusively offered by Verséa Ophthalmics, ocular surface disease patients, including Dry Eye Disease sufferers, can be diagnosed, treated, and monitored directly within your practice using quantitative IgE and lactoferrin results delivered within minutes.
Answer questions such as:
- What is the cause?
- Is it aqueous-deficient or evaporative disease?
- Is there an allergic component?
T-POC TESTING IS BILLABLE USING THE FOLLOWING UNIQUE CPT CODES:
Lactoferrin Test: CPT CODE 83520
IgE Allergy Test: CPT CODE 82785
Reimbursable by Medicare and Private Insurance*
*Verséa Ophthalmics does not guarantee reimbursement by any government or third-party payor